
Understanding the Quadratic Model of Pleasure and Pain
The Neuropsychoanalytic approach uses a quadratic equation to illustrate how human closeness regulates endogenous opioid tone. This equation, based on clinical observations, reflects how healthy individuals modulate their opioid tone through social interactions.
Equation:
Pleasure (x) = 4 – (x−3)^2 \]
x = Opioid Tone (limit \( x = 0 \) to \( x < 6 \))
Opioid Maintenance and Autism-Like Behavior
Patients maintained on high doses of opioids (such as buprenorphine) exhibit autistic-like behavior due to excessively high opioid tone (levels 5 to 6). This high tone inhibits the formation of therapeutic alliances because the pleasurable aspects of human contact become painful.
Key Points:
Opioid Maintenance Impact: Maintenance doses are significantly higher than what the brain naturally produces, leading to disengagement and discomfort in social interactions.
Therapeutic Alliance Challenges:
Opioid-maintained patients often find looking, talking, and touching painful, which disrupts the formation of therapeutic relationships.
Autism and the Neuropsychoanalytic Perspective
The "Three Hit" Model of Autism
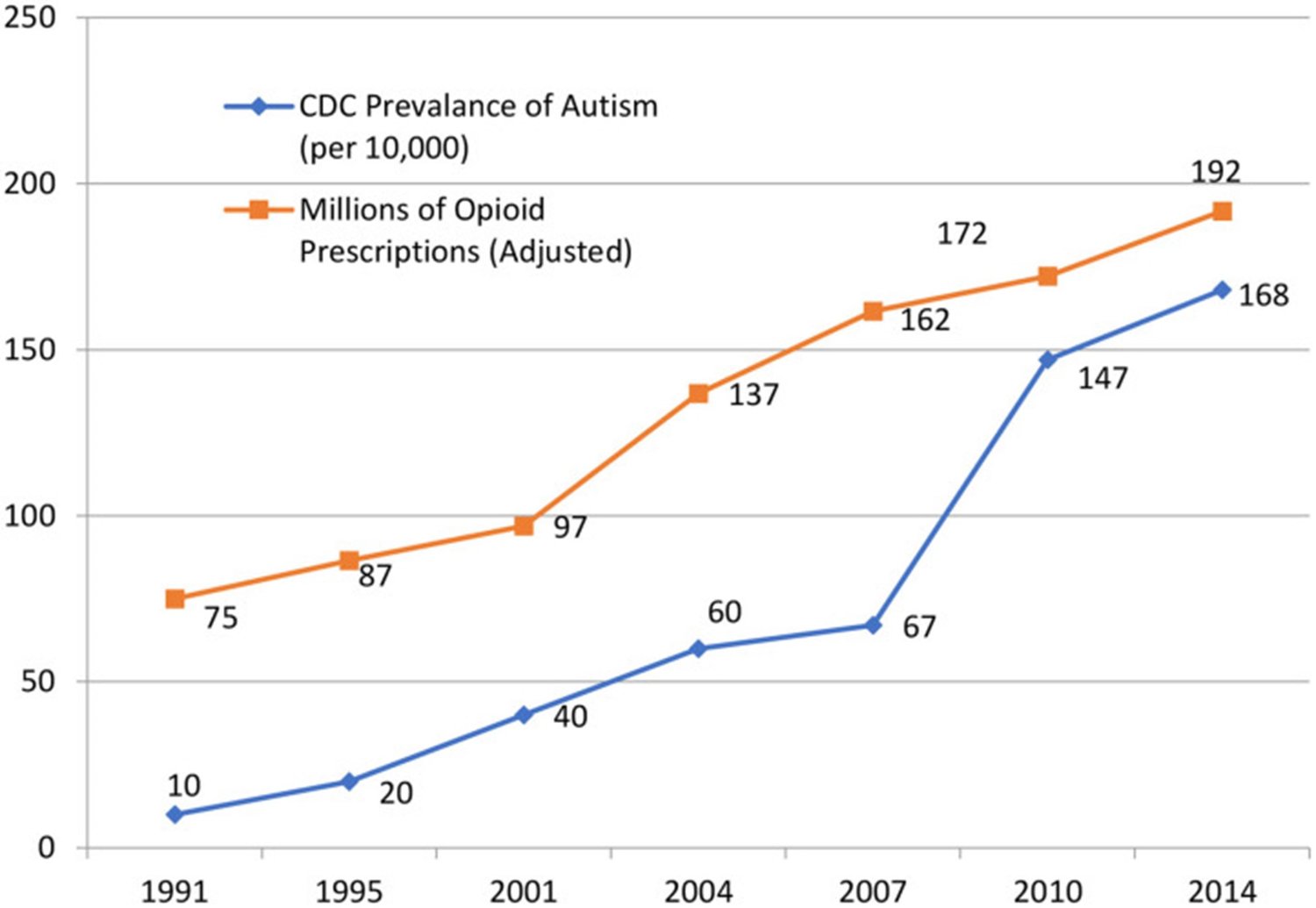
Autism’s increasing prevalence may be linked to a combination of genetic, environmental, and developmental factors:
1. Genetic Vulnerability: Specific genetic variants contribute to the development of autism.
2. Environmental Stressors: Events such as opioid administration during childbirth may interact with genetic vulnerabilities, potentially leading to autism.
3. Developmental Impact: This combination of factors can adversely affect neurodevelopment, contributing to the onset of autism. The graph shows our discovery of where the incidence of autism has been going up. Administration of opioids during labor/childbirth. (Johnson B, Ulberg S, Shivale S, Donaldson J, Milczarski B, Faraone SV. Fibromyalgia, autism, and opioid addiction as natural and induced disorders of the endogenous opioid hormonal system. Discov Med. 2014. 18:209-20.)
Autism and High Opioid Tone:
Social Withdrawal: High opioid tone causes discomfort during human interactions, leading to social withdrawal, gaze avoidance, and difficulties in speech mastery.
Parental Challenges: Parents may inadvertently cause pain through normal acts of love, leading to confusion and a disconnect in emp
Fibromyalgia: The Opposite of Autism
Just as autism may result from too much opioid tone, fibromyalgia could be caused by too little, making it an "opioid deficit disorder."
Fibromyalgia Characteristics:
Autoimmune Attack on Opioid Receptors: Fibromyalgia may involve an autoimmune process that damages mu opioid receptors, leading to symptoms like chronic pain, cold intolerance, and fatigue.
Overlap with Opioid Withdrawal Symptoms: Fibromyalgia symptoms closely resemble those of opioid withdrawal, suggesting a hormonal basis for the disorder.
Treatment with Low Dose Naltrexone (LDN)
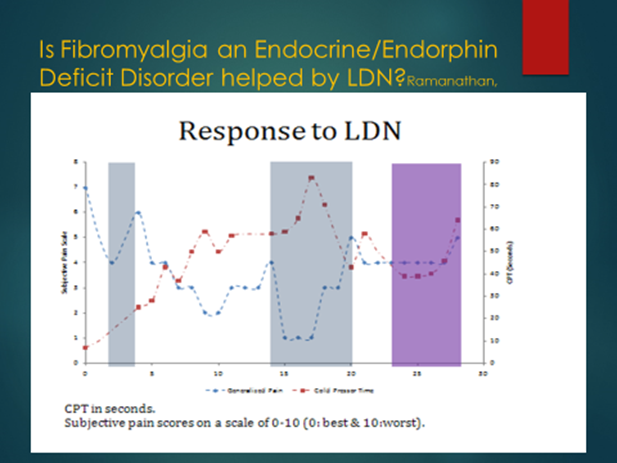
LDN has shown promise in treating both opioid-induced hyperalgesia (OIH) and fibromyalgia by enhancing opioid receptor function and reducing symptoms.
Key Findings:
Improved Pain Tolerance: Patients with fibromyalgia treated with LDN showed significant improvements in pain tolerance.
Dose Flexibility: Adjusting LDN dosage based on individual responses can optimize treatment outcomes.
Future Prospects: Ongoing research suggests that combining LDN with monoclonal antibodies could further improve treatment for fibromyalgia by preventing receptor destruction.
Relatedness and Psychiatric Disorders
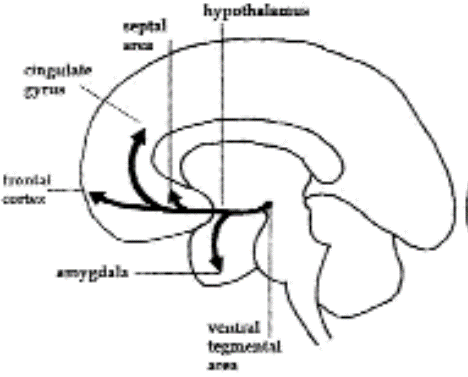
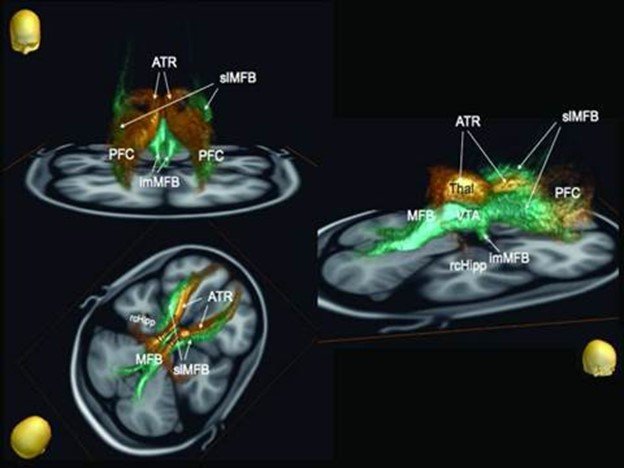
The lack of relatedness, driven by high opioid tone or disrupted SEEKING pathways, is a central factor in psychiatric disorders such as depression and addiction.
Key Concepts:
SEEKING Pathway Disruption: Drug addiction corrupts the SEEKING pathway, leading to mind control by drugs, where the will to use drugs overrides other drives.
Therapeutic Implications: Effective treatment requires restoring relatedness and managing the distressing emotions that arise when opioid use is discontinued.
Case Studies and Clinical Applications
Our clinical work demonstrates the practical application of these neuropsychoanalytic principles:
Chronic Pain Management: Detoxification from opioids, combined with psychotherapy, leads to improved pain management and reduced dependency.
Neonatal Abstinence Syndrome (NAS): Implementing neuropsychoanalytic contingency management in pregnant women on buprenorphine has dramatically reduced NAS incidence.
Learning from Observations: Systematic measurement of pain tolerance (CPT) and opioid use history allows for more accurate diagnosis and effective treatment of conditions like OIH and fibromyalgia.
References
1. Johnson B., Faraone SV. Outpatient detoxification completion and one month outcomes for opioid dependence. Neuropsychoanalysis 2013;15:145-60.
2. Anugu V, Ringhisen J, Johnson B. Case report, cause and treatment of “high opioid tone” autism. Frontiers in Psychology 2021. DOI: 10.3389/fpsyg.2021.657952.
Treatment with Low Dose Naltrexone (LDN)
Dr. Johnson has explored the use of Low Dose Naltrexone (LDN) for treating conditions like opioid-induced hyperalgesia (OIH) and fibromyalgia.
Detailed Observations:
Jaak Panksepp’s article on LDN had just been published when Upstate Addiction Medicine was opened. Dr. Johnson immediately began using LDN for opioid detoxification and subsequently for fibromyalgia, pairing it with the Cold Pressor Test (CPT). By measuring CPTs and following the response to LDN, Dr. Johnson discovered that OIH is a universal response to activating opioid receptors with exogenous opioid hormones like oxycodone or methadone.
With Institutional Review Board (IRB) informed consent permission, Dr. Johnson established normal CPTs by having 23 women and 23 men (who had no exposure to opioids or marijuana) serve as controls. The mean time for women was 111 seconds and for men was 114 seconds, showing that normal women have the same pain tolerance as normal men.
Case Example:
One fibromyalgia patient had severe pain that affected his entire body, including the soles of his feet. After starting LDN, his pain tolerance improved, and pain levels decreased. However, when LDN was stopped, the fibromyalgia symptoms returned, leading to a customized dosing regimen that improved his condition.
Learning by Counting: A Neuropsychoanalytic Approach
The Introduction of LDN and Cold Pressor Test (CPT)
When Dr. Jaak Panksepp's article on Low Dose Naltrexone (LDN) was published, Dr. Johnson immediately began applying LDN for opioid detoxification at Upstate Addiction Medicine. The approach was later extended to treat fibromyalgia, using the Cold Pressor Test (CPT) to measure the efficacy of LDN.
Key Findings:
OIH (Opioid-Induced Hyperalgesia): Dr. Johnson discovered that Opioid-Induced Hyperalgesia is a universal response to activating opioid receptors with exogenous hormones like oxycodone or methadone.
CPT as a Benchmark: Using the CPT, Dr. Johnson established normal pain tolerance benchmarks by involving 23 women and 23 men (who had no prior exposure to opioids or marijuana) as control subjects. The findings showed that women’s mean time was 111 seconds, and men’s was 114 seconds—statistically indistinguishable, indicating that normal women have the same pain tolerance as normal men.
Significantly Shorter CPT for Long-Term Opioid Users: The study showed that patients who used opioids long-term had significantly shorter CPTs, averaging 35 seconds for women and 54 seconds for men across 254 patients.
The Challenge of Recognizing OIH
Despite these findings, OIH remains under-recognized in the medical community. A 2022 paper, which polled pain experts, estimated OIH to occur in only 1 out of 10,000 patients—a rate so rare that it is often deemed insignificant. This contrasts with Dr. Johnson's findings, where objective measurements like CPT show a much higher prevalence.
Pain Experts' Approach:
Subjective vs. Objective Measures: Pain experts often rely on the Faces Pain Scale (FPS), a subjective measure, leading to different views on the frequency of OIH. Without recognizing the need to measure pain tolerance objectively, there is a risk that pain experts might increase opioid doses in response to the pain exacerbation caused by the medication, potentially leading to fatal overdoses.
The Role of LDN in Treating OIH
Dr. Johnson's research indicates that LDN can effectively reverse OIH, typically over three months. In contrast, gradual tapering of opioid medications often exacerbates pain as it is a withdrawal symptom, leading to increased risk of overdose deaths.
Key Statistics:
Overdose Risk with Tapering: In a study of 113,618 patients, those who had their opioid medications tapered experienced higher rates of overdose events and mental health crises. Specifically, tapering was associated with 9.3 overdose events and 7.6 mental health crises per 100 person-years, compared to 5.5 and 3.3 during non-taper periods.
LDN and Fibromyalgia
LDN has also shown promise in treating fibromyalgia, reducing pain, increasing energy, and even leading to remission of refractory depression in some cases.
CPT Findings in Fibromyalgia Patients:
Lower Starting CPT: Patients with fibromyalgia typically have lower starting CPTs, and the response to LDN shows less improvement, suggesting that there may be less opioid receptor function to recover.
Case Series:
Chronic Pain
Dr. Johnson followed 117 patients for a month after opioid detoxification. The outcomes were telling:66% of the patients remained off opioids.
Pain Levels: 51% reported improved pain levels, 46% saw no change, and 3% experienced worsened pain. This suggests that for 97% of the patients, opioids were primarily a source of side effects, with potentially fatal outcomes.
Neonatal Abstinence Syndrome (NAS)
Understanding the Challenges
Pregnancy is a complex time, particularly for women struggling with opioid addiction. While many pregnant women are committed to stopping all harmful substances, including tobacco, alcohol, and marijuana, those addicted to opioids often experience the opposite. Pregnancy can feel like another manifestation of their addiction, leading to increased drug use rather than cessation.
The MOTHER study, led by renowned expert Hendree Jones, provides valuable insights into the challenges faced by pregnant women on buprenorphine maintenance:
33% of women in the study dropped out of treatment.
85% continued using tobacco, despite receiving financial incentives for drug-free urine screens.
56% of neonates experienced NAS, requiring an average of 10 days in the hospital.
NAS, or Neonatal Opioid Abstinence Syndrome, is a heartbreaking condition. Newborns undergo withdrawal symptoms, including high-pitched crying, nasal congestion, hyperreflexia, and gut cramps, leading to dehydration. The detoxification process often involves the use of opioids like methadone and morphine.
The Neuropsychoanalytic Approach
Given these challenges, Dr. Johnson developed a neuropsychoanalytic contingency management psychotherapy to support pregnant women addicted to opioids. The primary goal of this approach is the birth of a healthy baby, achieved through a structured and supportive treatment plan:
Initial Visit Contract: The focus is on the baby’s health, and a support person, often the father or the patient's mother, is involved.
Educational Quiz: Patients take a quiz on the dangers of tobacco use during pregnancy, framed in a non-judgmental, playful manner. The reward for stopping drugs other than buprenorphine is the replacement of psychotherapy with check-in visits.
Treatment Schedule: Weekly meetings with urine drug screens (UDS) and carbon monoxide tests are conducted. If drug use persists, the frequency of meetings increases, eventually becoming daily if necessary.
Case Study Insights
Dr. Johnson’s approach has yielded impressive results:
Retention Rate: 84% of women remained in treatment, a rate higher than typically reported.
Substance Cessation: Almost all pregnant women stopped using other drugs, with tobacco being the last to go. In one case, a woman’s child had NAS due to her inability to quit clonazepam.
NAS Reduction: Transient NAS symptoms lasted less than a day, with the longest hospital stay being six days for monitoring, not treatment.
Key Discoveries
Dr. Johnson's research has led to several key discoveries:
Combined Withdrawal: What is commonly referred to as “neonatal opioid abstinence syndrome” is actually a combination of buprenorphine and nicotine withdrawal. Without tobacco use, there is no NAS.
Addressing Addiction Hostility
One of the critical challenges in treating opioid addiction during pregnancy is the hostility that often accompanies addiction. This hostility can be directed toward the fetus, manifesting as continued drug use, or toward the treatment providers. Dr. Johnson’s approach draws this hostility into the therapeutic relationship, where it can be safely managed without harming the fetus.
Conclusion
Dr. Johnson’s work integrates neuroscience with psychoanalysis, offering innovative treatments for addiction, autism, fibromyalgia, and other related disorders.
His insights into opioid tone regulation provide a comprehensive understanding of these complex conditions, leading to more effective and humane treatment approaches.
Detoxification Redefined
The term “detoxification” is outdated; instead, we focus on returning to homeostatic functioning. Understanding the neurochemical imbalances caused by substances like alcohol, benzodiazepines, and opioids is crucial for effective detoxification and recovery.
Alcohol Detoxification
Our approach to alcohol detoxification is outpatient-focused, using medications like valproic acid and chlordiazepoxide to manage withdrawal symptoms safely and effectively. This method is faster, safer, and more cost-effective than traditional inpatient detox, with a high completion rate and strong therapeutic alliances formed through the process. 78% completed outpatient detox in 3.5 hours or less. The completion rate was 97%. There were no seizures or delirium tremens despite severe withdrawal over 67 detoxes.
Benzodiazepine Detoxification
We use chlordiazepoxide, a long-acting benzodiazepine, to safely manage withdrawal symptoms. We don't "taper" chlordiazepoxide. We give ten 25 mg pills and let the patient take them as they like. The principle is that chlordiazepoxide has four active metabolites that mimic what alcohol does in the brain. Its functional half life is five days. This means that chlordiazepoxide builds up over several doses, eliminating the wish to take it frequently. Most patients take eight pills. Then the drug takes a month to leave the brain, giving a comfortable detox. Many people are admitted to the hospital for benzodiazepines detox. This approach is unique.
Opioid Detoxification
The key interventions are low dose naltrexone, which returns the opioid receptor system to normal by turning on opioid growth factor, and giving buprenorphine only once. No one else does opioid detox this way. This approach is unique and is supported by psychotherapy and close monitoring, leading to nearly 100% completion rates.
Key Concepts in Neuropsychoanalytic Addiction Treatment
The Role of Opioid Tone
Opioid tone refers to the activation level of opioid receptors in the brain, crucial for emotional regulation and social bonding. High-functioning individuals maintain an optimal opioid tone without external substances, while those with low opioid tone, often due to trauma, may turn to opioids to alleviate emotional pain.
Understanding Drug Use and Stigma
The goal of drug use in addiction is often misunderstood. It’s not merely about getting "high" but about achieving a semblance of normalcy despite severe emotional distress. Recognizing this shifts the perspective from blame to understanding, helping to address the root causes of addiction more effectively.
References
1. Johnson B, Mosri D. The neuropsychoanalytic approach: using neuroscience as the basic science of psychoanalysis. Frontiers in Psychology 2016;7. doi: 10.3389/fpsyg.2016.01459
2. Solms M., & Turnbull O. The Brain and the Inner World: An Introduction to the Neuroscience of Subjective Experience (1st ed.). Routledge. 2002
3. Panksepp J. Affective Neuroscience: The Foundations of Human and Animal Emotions. Oxford University Press. 1998.
References:
Outpatient Detoxification Outcomes:
The findings from Dr. Johnson’s study on outpatient detoxification completion and one-month outcomes for opioid dependence are based on his published work in Johnson B., Faraone SV. Outpatient detoxification completion and one-month outcomes for opioid dependence: A preliminary open-label study of a neuropsychoanalytic treatment. Neuropsychoanalysis 2013 .
Neuropsychoanalysis and Social Interaction:
The autoradiographic map and the effects of social interaction on the rat brain’s opioid system are detailed in Panksepp J, Bishop P. An autoradiographic map of (3H)diprenorphine binding in rat brain. Brain Res Bull. 1981 .
Autism and Endorphin Immunoreactivity:
The relationship between plasma beta-endorphin levels and autism, which supports the high opioid tone hypothesis, is from Leboyer M, Bouvard MP, Recasens C, et al. Difference between plasma N- and C-terminally directed beta-endorphin immunoreactivity in infantile autism. Am J Psychiatry. 1994 .
Drug Dreams and Neuropsychoanalytic Hypothesis:
Dr. Johnson’s hypothesis on drug dreams and their connection to the SEEKING system in the brain draws from Johnson B. A neuropsychoanalytic hypothesis. Journal of the American Psychoanalytic Association 2001 .
Fibromyalgia as an Endocrine Disorder:
The examination of fibromyalgia as a potential endocrine or endorphin deficit disorder, and the introduction of LDN as a treatment option, is discussed in Ramanathan S, Panksepp J, Johnson B. Is fibromyalgia an endocrine/endorphin deficit disorder? Psychosomatics 2012 .
LDN for Opioid-Induced Hyperalgesia and Fibromyalgia:
The use of Low Dose Naltrexone (LDN) for treating opioid-induced hyperalgesia and fibromyalgia is covered in Jackson D, Singh S, Zhang-James Y, Faraone S, Johnson B. The effects of low dose naltrexone on opioid-induced hyperalgesia and fibromyalgia. Frontiers in Psychiatry 2021 .
Cold Pressor Test and OIH:
The clinical utility of the Cold Pressor Test (CPT) in evaluating pain patients and treating opioid-induced hyperalgesia with LDN is documented in Oaks Z, Stage A, Middleton B, Faraone S, Johnson B. Clinical utility of the Cold Pressor Test: Evaluation of pain patients, treatment of opioid-induced hyperalgesia and fibromyalgia with low dose naltrexone. Discovery Medicine 2018 .
Buprenorphine Use in Pregnancy:
Tabi S, Heitner SA, Shivale S, Minchenberg S, Faraone SV, Johnson B. Opioid Addiction/Pregnancy and Neonatal Abstinence Syndrome (NAS): A Preliminary Open-Label Study of Buprenorphine Maintenance and Drug Use Targeted Psychotherapy (DUST) on Cessation of Addictive Drug Use. Front Psychiatry. 2020;11:563409.
SEEKING Pathway and Drug Dreams:
The detailed discussion on drug dreams as a reflection of a permanent change in the SEEKING pathway and REM sleep are controlled by different brain mechanisms. Johnson B. Drug dreams: a neuropsychoanalytic hypothesis. J Am Psychoanal Assoc. 2001;49:75-96.